Targeted Therapy Cost in India
About Targeted Therapy
What Is Targeted Therapy in Cancer Treatment?
Targeted therapy is a form of cancer treatment that utilizes drugs or other substances to identify and attack cancer cells while sparing most healthy cells. Unlike traditional chemotherapy, which affects rapidly dividing cells in general, targeted therapy works by interfering with specific molecules involved in cancer cell growth, progression, and survival.
These drugs are designed to "target" abnormalities in genes or proteins that are responsible for the uncontrolled division of cancer cells. By blocking these critical signals, targeted therapy can either stop the cancer from growing or eradicate the cancer cells. In some cases, it may help the immune system recognize and fight the tumor more effectively.
Targeted therapies are most commonly used in cancers such as:
- Breast cancer (HER2-positive)
- Lung cancer (EGFR or ALK mutations)
- Colorectal cancer (KRAS, BRAF mutations)
- Blood cancers like leukemia and lymphoma (CD20, BCL-2 targets)
- Kidney, liver, and thyroid cancers with specific gene markers
This form of treatment has revolutionized oncology, especially in advanced-stage cancers and relapsed cases, where standard treatments may no longer work. Targeted therapy can be given alone or in conjunction with chemotherapy, radiation, immunotherapy, or hormonal treatment, depending on the cancer type and stage.
Is Chemotherapy and Targeted Therapy the Same?
No, chemotherapy and targeted therapy are not the same, although both are used to treat cancer. Targeted and chemotherapy differ in how they work, how they are delivered, and how they affect the body.
Targeted Therapy
Targeted therapy is designed to precisely attack cancer cells by focusing on specific genes, proteins, or other molecules that help the cancer grow or spread. These drugs do not harm most healthy cells and are chosen based on the unique molecular profile of the patient's tumor.
- Precision-focused
- Fewer side effects
- Personalized for the cancer type
- Works best when a known mutation is present
- Can be given as pills or IV infusions
Chemotherapy
Chemotherapy, on the other hand, is more general. It attacks all fast-growing cells, whether they are cancerous or healthy. It includes cells in the hair, digestive tract, and bone marrow, which is why chemotherapy often causes more side effects like hair loss, nausea, and fatigue.
- Non-specific attack
- More likely to damage healthy tissues
- Used for a broad range of cancers
- Typically delivered via IV or injection
Key Difference
Think of it like this: Chemotherapy is like using a shotgun, while targeted therapy is like using a laser pointer. Both can be effective, but targeted therapy is usually preferred when the cancer has a specific mutation that can be exploited. In many treatment plans, doctors may combine both approaches to increase effectiveness, especially in aggressive or advanced cancers.
How Does Targeted Therapy Work?
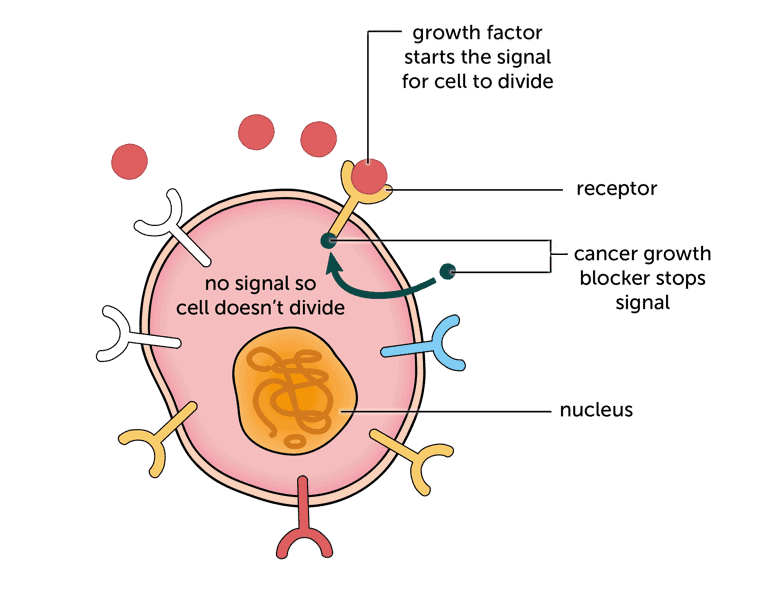
Targeted therapy works by interfering with certain genes, proteins, or the tissue environment that helps cancer cells grow and survive. These drugs are engineered to recognize cancer cells based on specific biological markers and then block the signals they use to multiply or spread.
The process begins with identifying molecular targets, which are abnormalities or mutations found in cancerous cells but not in normal ones. Once these targets are identified through genetic or biomarker testing, oncologists choose a drug that precisely blocks or alters the function of those targets.
Targeted therapy works in different ways:
- Blocking cell growth signals: Some drugs stop the signals that tell cancer cells to grow uncontrollably.
- Triggering cell death (apoptosis): Certain therapies activate internal mechanisms that lead cancer cells to self-destruct.
- Cutting off blood supply (angiogenesis inhibition): Some agents stop the formation of new blood vessels, starving the tumor of nutrients.
- Marking cancer cells for destruction: Monoclonal antibodies may flag cancer cells so the immune system can recognize and destroy them.
- Delivering cytotoxic substances directly to cancer cells: Some drugs carry radioactive particles or toxins directly into the tumor.
What are the Different Types of Targeted Therapy Used?
Oncologists use a broad spectrum of targeted therapies that align with global treatment standards. Each type works on specific cancer-driving mechanisms, making treatment more precise and tailored to individual patients.
Here are the most common forms of targeted therapies available in cancer centers:
Monoclonal Antibodies (mAbs)
These are lab-made antibodies that mimic the immune system. They latch onto specific proteins found on the surface of cancer cells, blocking their function or marking them for immune destruction. Some also deliver chemotherapy or radioactive agents directly into the cancer cells.
Examples: Trastuzumab (HER2-positive breast cancer), Rituximab (B-cell lymphoma), Cetuximab (colorectal cancer)
Tyrosine Kinase Inhibitors (TKIs)
TKIs are small molecules that enter cancer cells and block enzymes called tyrosine kinases, which are involved in transmitting growth signals. By disrupting these signals, the drugs stop or slow down tumor development.
Examples: Imatinib (CML), Erlotinib (EGFR-positive lung cancer), Sunitinib (kidney cancer)
Angiogenesis Inhibitors
These medicines prevent the formation of new blood vessels that tumors need to grow. By cutting off the supply of oxygen and nutrients, the tumor cells gradually shrink or stop spreading.
Example: Bevacizumab (used in colorectal, lung, and ovarian cancer)
mTOR and PARP Inhibitors
These are newer classes of targeted agents that block proteins involved in cell repair and growth. PARP inhibitors, in particular, have shown strong results in BRCA-mutated ovarian and breast cancers.
Examples: Everolimus (mTOR), Olaparib (PARP)
Proteasome Inhibitors
Used mainly in blood cancers like multiple myeloma, these drugs block cellular machinery responsible for breaking down proteins, causing cancer cells to accumulate waste and die.
Example: Bortezomib
Immunotargeted Therapies (Biological Response Modifiers)
These are hybrid therapies that both target cancer-specific markers and boost the immune system's response. They are especially valuable in advanced or relapsed cancers.
When Is Targeted Therapy Recommended?
Targeted therapy is carefully prescribed when a tumor carries specific genetic mutations or protein markers that can be "targeted" by particular drugs. Before starting treatment, doctors run molecular or biomarker tests to check whether the cancer expresses these targets.
Targeted therapy is usually recommended in the following situations:
- When Cancer Has Specific Genetic Mutations: If testing reveals a mutation such as EGFR in lung cancer or HER2 in breast cancer, targeted drugs become the first line of defense.
- When Standard Chemotherapy Has Limited Effectiveness: In many cases, if the tumor does not respond well to conventional chemotherapy or if the cancer returns after initial treatment, targeted therapy is introduced to halt further progression.
- When Precision Treatment Is Required for Better Tolerability: Targeted therapy is often used when a patient cannot tolerate aggressive chemotherapy. Since it works selectively, it causes less damage to healthy cells and is usually better tolerated, especially in elderly or frail patients.
- When Cancer Has Spread (Metastatic Stage): Doctors recommend targeted therapy in advanced or metastatic cancers where the goal is to prolong life, reduce symptoms, and maintain quality of life. Many such patients respond well when their treatment is matched with the tumor's unique biology.
- In Maintenance or Adjuvant Settings: Some patients receive targeted drugs after initial treatment (such as surgery or chemotherapy) to reduce recurrence risk. It is often seen in leukemia or breast cancer protocols.
Is Targeted Therapy Available for All Types of Cancer?
No, targeted therapy is not available for all types of cancer. It is only effective when a tumor has specific genetic mutations or protein markers that targeted drugs can act upon. That's why molecular testing is crucial. It tells the doctor whether your cancer has a "target" that a drug can hit.
Where Targeted Therapy Works Well
It is most commonly used in cancers like:
- Non-small cell lung cancer (EGFR, ALK, ROS1 mutations)
- Breast cancer (HER2-positive)
- Colorectal cancer (KRAS/BRAF wild-type)
- Chronic myeloid leukemia (Philadelphia chromosome)
- Lymphomas (CD20-positive B-cell lymphomas)
- Kidney, liver, ovarian, and thyroid cancers with actionable mutations
When It's Not Suitable
If your cancer doesn't carry a known mutation or protein expression that matches an available drug, targeted therapy will likely be ineffective. In such cases, chemotherapy, immunotherapy, or radiation may be recommended instead.
Targeted therapy is not based on cancer type alone. It's based on the biological makeup of the tumor. Two patients with the same cancer might need completely different treatments depending on their tumor's genetic profile.
How Do Oncologists Decide if Targeted Therapy Will Work for You?
Before initiating targeted therapy, doctors must confirm whether a patient's tumor contains specific mutations or protein expressions that can be effectively treated with targeted drugs. It requires precise and advanced diagnostic tests, which form the foundation of a personalized treatment plan.
- Molecular Testing (Genetic Mutation Analysis): This is the most critical test. Using a tissue sample from a biopsy, laboratories check for specific mutations like EGFR, ALK, KRAS, HER2, BRAF, or BRCA, depending on the cancer type. It helps doctors match the right drug to the patient's tumor profile.
- Immunohistochemistry (IHC): IHC testing involves staining the tumor tissue to detect the presence or overexpression of specific proteins on the cancer cell surface. It is widely used for HER2, PD-L1, and CD markers in solid tumors and lymphomas.
- Fluorescence In Situ Hybridization (FISH): FISH is a specialized test used to detect chromosomal abnormalities and gene rearrangements. It's often recommended for ALK-positive lung cancers or HER2 amplification in breast cancer when IHC results are ambiguous.
- Next-Generation Sequencing (NGS): NGS offers a broader view by screening multiple genes at once. This test is beneficial in complex cases where more than one mutation might be driving the cancer. It's increasingly being used in India for advanced-stage or treatment-resistant cancers.
- Liquid Biopsy (Optional): When a tumor is not easily accessible or biopsy isn't possible, a blood-based test (liquid biopsy) may be done to detect DNA fragments from cancer cells circulating in the bloodstream.
- Routine Blood Tests and Organ Function Panels: These tests evaluate liver, kidney, and bone marrow function to ensure the patient can safely tolerate targeted therapy drugs.
Send Query
About Targeted Therapy in India
What is the Treatment Protocol for Targeted Therapy in India?
In India, the protocol for delivering targeted therapy follows a stepwise, evidence-based approach, combining global treatment guidelines with personalized care. The process begins with confirming if the patient's cancer is eligible for targeted treatment based on molecular characteristics.
- Diagnostic Workup: The journey starts with advanced testing. Doctors order molecular profiling, genetic sequencing, and immunohistochemistry to identify specific markers or mutations like EGFR, ALK, HER2, or BRAF.
- Multidisciplinary Case Review: A tumor board, typically including a medical oncologist, pathologist, radiologist, and molecular biologist, reviews the test results to confirm whether targeted therapy is the right fit for the case.
- Drug Selection Based on Mutation Type: Once a target is confirmed, oncologists prescribe an appropriate drug. The choice may depend on factors like drug availability (original vs. biosimilar), patient age, comorbidities, and past treatment responses.
- Initiation of Treatment: The therapy is administered in either of two ways:
- Oral tablets/capsules: Taken at home under supervision (e.g., TKIs)
- IV infusions in daycare centers: Given in hospital settings (e.g., monoclonal antibodies)
- Each cycle may last 3–4 weeks, and the total number of cycles varies depending on how the patient responds.
- Monitoring and Follow-Up: Patients undergo regular imaging (PET-CT, MRI) and blood tests to evaluate tumor response. Dose adjustments or drug switching may be done if the cancer stops responding or side effects appear.
- Long-Term Maintenance or Transition: If the tumor responds well, doctors may continue maintenance therapy for several months or years. If resistance develops, alternative targeted agents or combination therapies are explored.
Targeted Therapy Cost in India
The cost of targeted therapy in India typically ranges between ₹1,50,000 to ₹4,00,000 ($1,800 to $4,800) per cycle, depending on several factors such as the type of drug, the cancer being treated, and the duration of treatment. Some patients may require just a few cycles, while others (especially those on maintenance therapy) may continue for several months or even years.
Some of the factors that influence the price are:
- Type of Targeted Drug: Branded drugs like Trastuzumab, Bevacizumab, or Osimertinib can be expensive, while biosimilar versions reduce the cost significantly without compromising quality.
- Cancer Type and Mutation: A therapy for HER2-positive breast cancer may cost less per cycle than a drug used in lung cancer with an ALK mutation.
- Cycle Duration and Frequency: Most treatments follow 21-day or 28-day cycles, and the total cost increases with more cycles.
- Mode of Administration: Oral drugs are often cheaper than intravenous (IV) infusions, which also incur administration and daycare charges.
- Hospital Category: Treatment at premium cancer centers in metro cities may cost more due to high-end infrastructure and services.
Cancer Type | Drug Type Example | Approx. Cost Per Cycle (INR) | Cost in USD |
| Breast Cancer (HER2+) | Trastuzumab | ₹1,80,000 – ₹2,80,000 | $2,200 – $3,300 |
| Lung Cancer (EGFR/ALK+) | Osimertinib / Crizotinib | ₹2,00,000 – ₹4,00,000 | $2,400 – $4,800 |
| Colorectal Cancer (KRAS wild-type) | Cetuximab / Bevacizumab | ₹1,50,000 – ₹2,50,000 | $1,800 – $3,000 |
| CML / Leukemia | Imatinib / Dasatinib | ₹50,000 – ₹1,20,000 | $600 – $1,450 |
| Kidney / Liver Cancer | Sunitinib / Sorafenib | ₹90,000 – ₹1,80,000 | $1,100 – $2,200 |
Note: These prices are indicative. Drug prices vary based on brand vs. biosimilar, import status, and hospital markup.
What's Included in the Targeted Therapy Package?
When receiving targeted therapy in India, patients often benefit from comprehensive care packages that cover far more than just the medication. These packages are designed to streamline treatment and eliminate hidden expenses, making it easier for patients and caregivers to plan financially.
Standard inclusions in a targeted therapy treatment package are:
- Oncology Consultations
- Pre-Treatment Investigations
- Daycare Drug Administration (If IV-based)
- Medication Cost (One Cycle)
- Daycare or Short Hospital Stay (if required)
- Follow-Up Review and Reports
Cost Breakdown of Targeted Therapy in India
The total cost of targeted therapy depends on multiple components that go beyond the drug itself. Below is a detailed breakdown of what contributes to the overall expense of each cycle:
- Initial Oncology Consultation: Before therapy begins, patients undergo a thorough review with an oncologist. It helps assess medical history, current condition, and treatment suitability. This consultation usually costs between ₹2,000 to ₹5,000 ($25–$60).
- Genetic and Biomarker Testing: Since targeted therapy is based on specific mutations, the cost of molecular diagnostics like EGFR, ALK, HER2, or NGS panels is a critical part of the initial workup. These tests can cost ₹20,000 to ₹60,000 ($240–$720), depending on the complexity.
- Drug Cost Per Cycle: This is the most expensive component. Branded targeted drugs range between ₹1,20,000 and ₹3,50,000 ($1,450–$4,200) per cycle, though biosimilars may cost less.
- Administration Charges: For intravenous drugs, daycare, or infusion charges are added. It typically costs ₹5,000 to ₹10,000 ($60–$120) per cycle.
- Supportive Medications and Monitoring – Anti-allergy medications, antiemetics, and organ monitoring tests are often required during each cycle and may cost an additional ₹5,000 to ₹15,000 ($60–$180).
- Follow-Up Consultations and Imaging: Post-treatment reviews, scans (CT, PET-CT), and lab tests are done periodically to evaluate the effectiveness of the therapy. These may add ₹8,000 to ₹20,000 ($100–$240) across the treatment duration.
Cost Component | Estimated Cost (INR) | Estimated Cost (USD) |
| Initial Consultation | ₹2,000 – ₹5,000 | $25 – $60 |
| Genetic/Biomarker Testing | ₹20,000 – ₹60,000 | $240 – $720 |
| Targeted Drug (Per Cycle) | ₹1,20,000 – ₹3,50,000 | $1,450 – $4,200 |
| Daycare/Infusion Charges | ₹5,000 – ₹10,000 | $60 – $120 |
| Supportive Medicines & Monitoring | ₹5,000 – ₹15,000 | $60 – $180 |
| Follow-up and Imaging | ₹8,000 – ₹20,000 | $100 – $240 |
Total Estimated Cost Per Cycle: ₹1,60,000 – ₹4,60,000 ($1,950 – $5,500)
Cost Comparison: India vs Other Countries
Targeted cancer therapy is often prohibitively expensive in many developed countries. In contrast, India offers the same FDA-approved drugs, internationally trained oncologists, and advanced hospital facilities at a significantly reduced cost, making it a global hub for affordable precision oncology.
The table below compares the average cost per cycle of targeted therapy across countries:
Country | Average Cost Per Cycle (USD) | Inclusions |
| India | $1,800 – $4,800 | Drug cost, oncologist consultation, diagnostics, daycare charges, follow-up |
| United States | $10,000 – $25,000+ | Drug only; excludes hospital stay and diagnostics in most cases |
| United Kingdom | $8,000 – $20,000 (Private Care) | Drug + consultation; NHS options are limited to UK residents |
| Canada | $9,000 – $18,000 | Public care is often restricted to citizens; private care is expensive |
| UAE/Middle East | $7,500 – $15,000 | Includes branded drugs and hospital stay; higher cost due to import pricing |
| Singapore | $6,000 – $12,000 | Advanced care, but overall cost is 2–3x that of India |
| Thailand | $4,000 – $8,000 | Lower cost than the West, but still higher than India for long-term treatment |
Why India Is More Affordable:
- Access to cost-effective biosimilars
- Local manufacturing of key oncology drugs
- Competitive pricing in private hospitals
- Lower consultation and hospital overheads
- Government-regulated drug pricing policies for life-saving medications
Despite the price advantage, India doesn't cut corners. Hospitals maintain international accreditation, use the same treatment protocols as in the US/UK, and are staffed with globally trained oncologists.
What Services are Available for International Cancer Patients in India?
India has become a preferred destination for targeted cancer therapy among international patients, thanks not just to its medical affordability, but also its end-to-end patient support system. From the moment you express interest in treatment, dedicated medical teams and coordinators work to simplify your journey.
- Hassle-Free Arrival Support: Patients receive airport pick-up services, fast-tracked medical visas, and help with travel logistics, including flight booking, ambulance transfers (if needed), and local transportation during treatment.
- Personalized Hospital Assistance: Dedicated International Desks handle everything from appointments to billing. Language interpreters (Arabic, Russian, French, and others) ensure clear communication. Patients are assigned treatment coordinators who stay in touch 24/7 for any queries.
- Affordable Accommodation Options: Hospitals often partner with nearby guesthouses, serviced apartments, and hotels to offer clean and affordable accommodation for patients and their families during extended treatments like targeted therapy.
- Medical Documentation and Visa Support: Assistance with medical visa letters and embassy documents. Help with compiling and translating medical reports for pre-arrival evaluation.
- Post-Treatment Follow-Up from Abroad: Many hospitals offer online follow-up consultations with oncologists, so patients don't need to travel back unless necessary. Scans and blood reports can be reviewed digitally with the medical team.
- Emotional and Nutritional Support: Some cancer centers also offer psychological counseling, dietary guidance, and access to patient communities to support holistic healing during therapy.
Is Targeted Therapy Covered by Insurance or Government Schemes?
Targeted therapy is often one of the costliest components of cancer care, which raises a crucial question: Does insurance or government support in India cover it? The answer depends on the type of insurance policy and the patient's eligibility for public schemes.
Private Health Insurance
Most comprehensive health insurance plans in India now cover targeted therapy under their inpatient hospitalization benefit or daycare procedures. However, patients must ensure:
- The policy does not have a cap on chemotherapy or cancer treatment expenses.
- The specific drug prescribed is listed in the insurer's formulary.
- Pre-authorization is obtained before beginning the treatment.
Some insurers may partially cover the cost of the drug and fully cover administration, diagnostics, and hospitalization. It's essential to read the fine print and confirm inclusions with the provider.
Employee/Corporate Insurance Policies
Employees covered under group medical insurance through their company often receive broader coverage for cancer therapies, including targeted therapy. However, limits and co-pay clauses may apply.
Government Schemes (for Indian Citizens)
Several national and state-run schemes offer assistance for economically weaker sections:
- Ayushman Bharat – PM-JAY: Covers certain cancers and therapies, but access to high-cost targeted drugs is limited under standard packages.
- State Health Schemes: Some states provide financial aid through programs like Arogyasri (Telangana/AP), Karunya (Kerala), and CM Relief Funds.
- NGO and Hospital-Based Support: Select hospitals and cancer NGOs in India offer patient assistance programs, donor support, or drug discounts for eligible low-income patients.
For International Patients
International medical tourists generally do not qualify for Indian government subsidies. However, hospitals often negotiate special rates, offer generic/biosimilar alternatives, and tailor therapy plans based on budget without compromising care quality.
What is the Success Rate of Targeted Therapy in India?
The success of targeted therapy largely depends on how accurately the treatment is matched to the patient's cancer profile. In India, leading cancer centers have achieved high response rates and longer survival outcomes, especially when therapy is guided by genetic and molecular testing.
Because targeted therapy is designed to block the specific mechanisms that drive tumor growth, it often works faster and more effectively than conventional treatments in eligible patients.
Success rates vary by cancer type, stage, and mutation. But when used appropriately, results are impressive:
- Non-Small Cell Lung Cancer (EGFR/ALK mutations): 60%–80% of patients show a major response; many achieve stable disease for 12–24 months.
- HER2-Positive Breast Cancer: Over 50% of patients experience tumor shrinkage; with combined treatments, 5-year survival improves significantly.
- CML (Chronic Myeloid Leukemia): Over 90% of patients respond well to TKIs like imatinib, with many entering long-term remission.
- Colorectal Cancer (KRAS wild-type): Patients treated with EGFR inhibitors often show prolonged progression-free survival.
- Lymphoma (CD20+ B-cell): Rituximab-based therapies have drastically improved remission and relapse-free periods.
Factors Behind India's Success in Targeted Therapy:
- Accurate diagnostics: Molecular profiling ensures the right drug is chosen from the start.
- International treatment protocols: Hospitals follow NCCN, ESMO, and ASCO guidelines.
- Access to biosimilars and FDA-approved originals: Enables continuous, uninterrupted therapy.
- Multidisciplinary teams: Oncologists, pathologists, and radiologists work together to monitor progress.
Note: Targeted therapy may not "cure" advanced cancers in every case, but it often halts progression, reduces tumor burden, and improves quality of life. In some cases, it converts inoperable tumors into operable ones or prepares the body for further curative treatments.
Recovery and Monitoring After Targeted Therapy
Recovery after targeted therapy doesn't always follow the same path as chemotherapy. Since these drugs are designed to act selectively on cancer cells, patients often experience a more manageable recovery period. However, close monitoring is essential to track effectiveness and manage side effects.
Most patients undergoing targeted therapy in India remain active and continue their daily routines. It is especially true for oral therapies taken at home. Unlike chemotherapy, there's usually no hair loss, intense nausea, or severe fatigue.
Regular Monitoring Is Crucial
Doctors closely monitor patients during and after each cycle. It includes:
- Blood Tests: To evaluate organ function (mainly liver and kidneys) and detect early signs of toxicity.
- Imaging Scans: CT, MRI, or PET-CT scans are done periodically to assess whether the tumor is shrinking or staying stable.
- Mutation Reassessment: In cases where the cancer becomes resistant, additional molecular testing may be done to switch to a second-line targeted drug.
- Symptom Check-ins: Oncologists review symptoms like rash, diarrhea, elevated blood pressure, or fatigue to adjust dosages if needed.
Duration of Recovery
Recovery time varies. For patients on short-term targeted therapy, recovery can begin within weeks after stopping treatment. For maintenance or long-term therapy, side effects may be mild, but continuous monitoring is needed over months or years.
Targeted Therapy Cost Comparison by Country
Compare Targeted Therapy costs across different countries to make an informed decision about your medical treatment.
| Country | Cost Range (USD) | Potential Savings | Action |
|---|---|---|---|
INIndiaCurrentBest Value | $1,800 - $4,800 | — | Get Quote |
Note: Costs may vary based on hospital choice, room type, additional services, and individual medical requirements. Contact us for a personalized quote.
Leading Hospitals for Targeted Therapy in India

SP Medifort Hospital
SP Medifort, Thiruvananthapuram, is a JCI-accredited, 475-bed multi-super-specialty hospital spread across 500,000 sq. ft. The hospital houses 10 modu...
Accreditations


Facilities

CARE Hospitals, Banjara Hills, Hyderabad
CARE Hospitals, Banjara Hills, Hyderabad, is a 435-bed NABH and NABL-accredited multispecialty hospital with 120 critical care beds. Established in 20...
Accreditations

Facilities

AIG Hospitals, Gachibowli, Hyderabad
AIG Hospitals, Gachibowli, Hyderabad, is a 1,000-bed, JCI- and NABH-accredited super-specialty hospital spanning 1.7 million sq. ft. It is the flagshi...
Accreditations


Facilities

Gleneagles Global Health City, Chennai
Gleneagles Global Health City, Chennai, is a 200-bed quaternary-care hospital and part of the IHH Healthcare network, one of the world’s largest priva...
Accreditations

Facilities

MGM Healthcare, Chennai
MGM Healthcare, Chennai, is a 400-bed quaternary-care super-specialty hospital accredited by JCI, NABH, and NABL. The hospital features 100 ICU beds,...
Accreditations


Facilities

MIOT International, Chennai
MIOT International, Chennai, is a 1,000-bed NABH- and NABL-accredited multispecialty hospital serving patients from more than 130 countries. Establish...
Accreditations

Facilities

Apollo Hospitals, Greams Road, Chennai
Apollo Hospitals, Greams Road, Chennai, is the flagship hospital of the Apollo Group. Established in 1983, it has 560 beds, 46 ICUs, and 15 operating...
Accreditations



Facilities

HCG Cancer Centre, Mumbai
HCG Cancer Centre, Borivali, Mumbai, is an NABH- and AACI-accredited comprehensive cancer hospital established in 2019. The 119-bedded facility includ...
Accreditations


Facilities

Apollo Hospitals, Navi Mumbai
Apollo Hospitals, Navi Mumbai, established in 2016, is a 500-bed JCI- and NABH-accredited quaternary care hospital offering advanced treatment across...
Accreditations


Facilities

Marengo Asia Hospitals, Faridabad
Marengo Asia Hospital, formerly QRG Health City, is a 325-bed NABH and NABL-accredited multispecialty hospital in Faridabad. It offers advanced care i...
Accreditations

Facilities
FAQ
Browse by Department
Explore procedures in different departments
Related Procedures
Other procedures in this department
Get a Free Treatment Plan
Our website uses cookies. By clicking on accept you give your consent to the use of cookies as per our Privacy Policy.